Intertan Intramedullary Nail Features
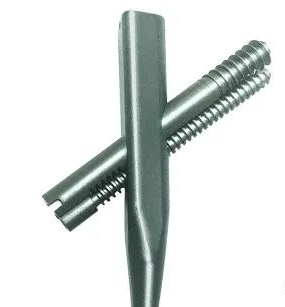
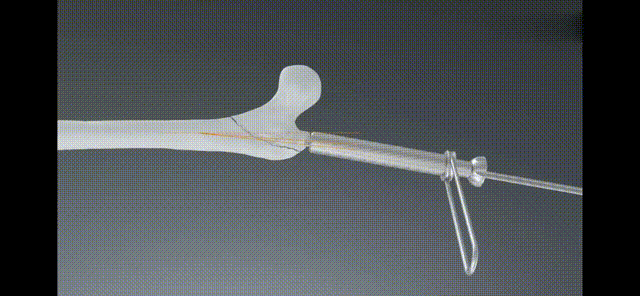
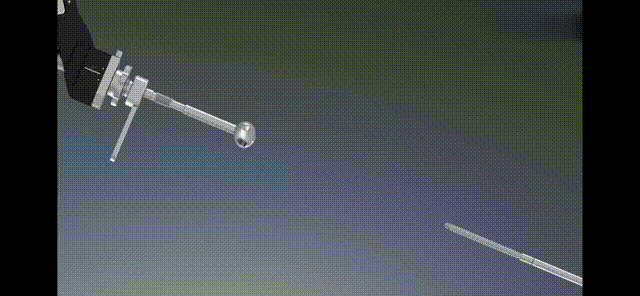
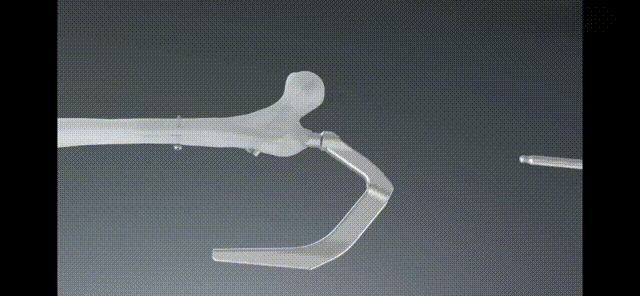
In terms of head and neck screws, it adopts a double-screw design of lag screws and compression screws. The combined interlocking of 2 screws enhances the resistance to rotation of the femoral head.
During the process of inserting the compression screw, the axial movement of the lag screw is driven by the occlusal thread between the compression screw and the lag screw, and the anti-rotation stress is transformed into linear compression on the fracture end, thereby significantly enhancing the anti-rotational force of the screw. Cut out performance. The 2 screws are jointly interlocked to avoid the "Z" effect.
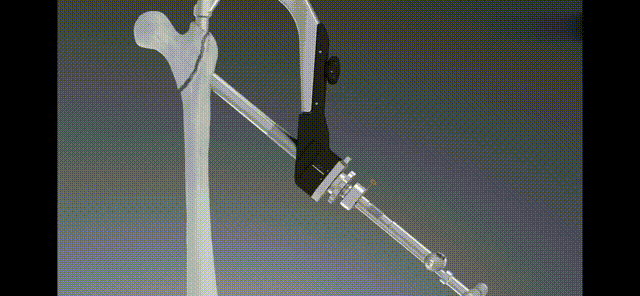
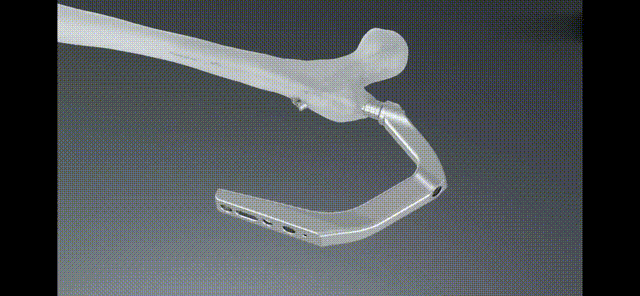
The design of the proximal end of the main nail similar to that of a joint prosthesis makes the nail body more compatible with the medullary cavity, and more in line with the biomechanical characteristics of the proximal femur.
Surgical Steps
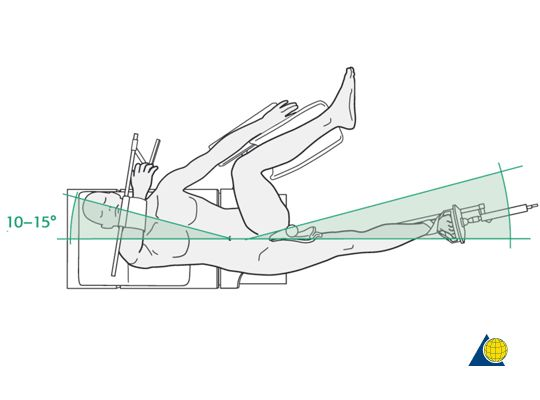
Position: The patient can choose lateral or supine position. With the patient in the supine position, on a radiolucent operating table or orthopedic traction table. The healthy side of the patient is adducted and fixed on the bracket, and the affected side is adducted 10°-15° to facilitate alignment with the medullary cavity.
Accurate reset: Traction the affected limb with the traction bed before operation, and adjust the traction direction under fluoroscopy so that the affected limb is in a slight internal rotation and adduction position. Most fractures can be reset well. Preoperative reset is very important and The point is, don’t cut it easily if there is no satisfactory reduction. This can save the operation time and reduce the difficulty during the operation. If the reduction is difficult, you can make a small incision during the operation and use the push rod, retractor, reduction forceps, etc. to assist the reduction. Minor fractures The inner and outer sides are separated, and there is no need to adjust repeatedly. The fracture end can be automatically reset when the compression screw is screwed in during the operation.
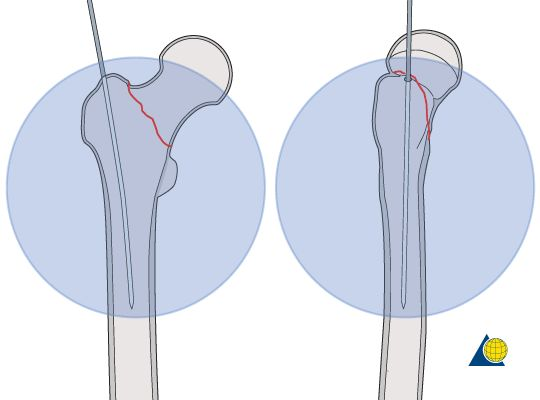
Reduction of the lesser trochanter: The design of the intramedullary nail does not require the continuity of the medial cortex. Generally speaking, there is no need to reduce the lesser trochanter fracture fragment, because the minimally invasive closed reduction operation has less impact on the blood circulation of the fracture end, and the fracture is easy to heal. However, the coxa varus should be corrected before the screw is placed, and the time of going to the ground and postoperative weight-bearing time should be delayed appropriately
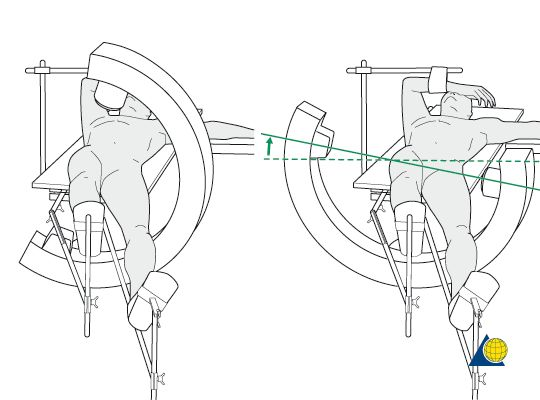
Incision position: A 3-5 cm longitudinal incision is made at the proximal end of the greater trochanter apex approximately at the level of the anterior superior iliac spine. A Kirschner wire can be placed on the outer side of the proximal femur, and adjusted to be consistent with the long axis of the femur under C-arm fluoroscopy, so that the positioning of the incision is more accurate.
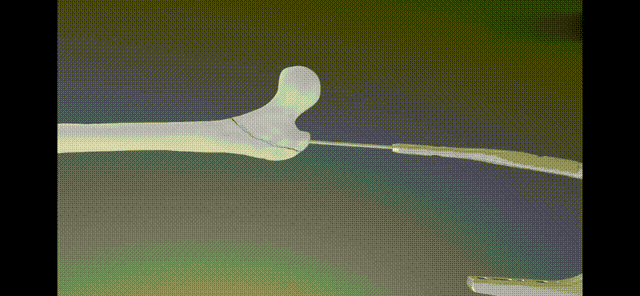
Determine the entry point: the entry point is slightly medial to the apex of the greater trochanter, which corresponds to a 4° lateral deviation of the long axis of the medullary cavity on the frontal view. On the lateral view, the nail entry point is located on the long axis of the medullary cavity;
Needle Entry Point

Insert Guide Pin Fluoroscopy
Fully Reamed
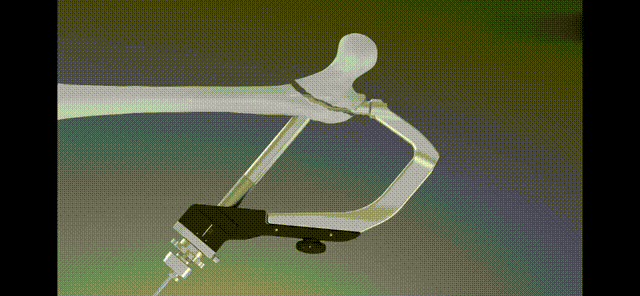
Since the proximal end of the InterTan main nail is relatively thick, the nail can only be inserted after full reaming during the operation. The proximal reaming should be stopped when the restricting device of the reaming drill touches the entry channel tool. Whether the distal femoral shaft is reamed depends on the The size of the medullary cavity is determined. If the preoperative X-ray finds that the medullary cavity of the proximal femoral shaft is obviously narrow, the femoral shaft reamer should be prepared before the operation. If the reaming is not sufficient, it will make it difficult to insert the screw. During the process of screwing, it may shake in a small range The lateral components of the intramedullary nail should be avoided, but violent knocking on the nail tail should be avoided. Such rough knocking may easily cause bone splitting during the operation or redisplacement of the fracture after reduction.
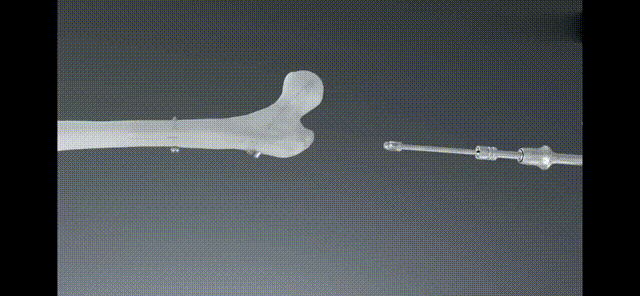
Insert the soft tissue protection sleeve, drill in along the guide wire with a drill, and expand the proximal femoral channel for the intramedullary nail (above picture); if the medullary cavity is narrow, use the reamed soft drill to expand the medullary cavity to an appropriate width; connect the guide insert the InterTAN main nail into the medullary cavity (below);
Proximal Lock
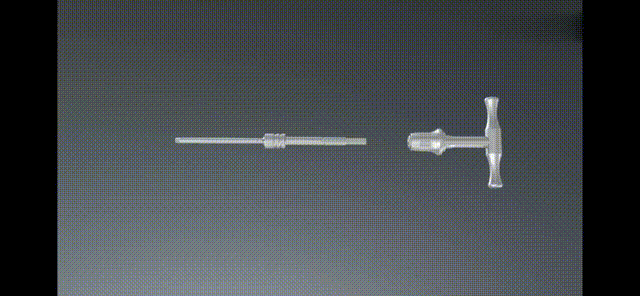
Lag screw placement
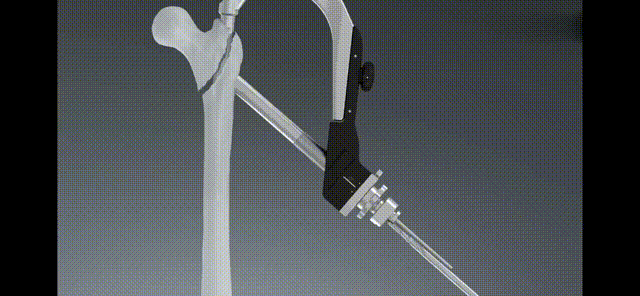

Compression screw placement
Screw in the distal locking nail

Remote Lock
End Cup
Postoperative Treatment
Antibiotics were routinely used to prevent infection 48 hours after the operation; low-molecular-weight heparin calcium and air pumps were used to prevent deep vein thrombosis (DVT) in the lower extremities, and basic medical diseases were continued to be treated. Plain radiographs of the pelvis and anteroposterior and lateral radiographs of the affected hip joint were routinely taken to understand fracture reduction and internal fixation.
On the first day after surgery, the patient was encouraged to perform isometric contraction of the quadriceps femoris in a semi-recumbent position. On the second day, the patient was instructed to sit on the bed. On the third day, the patient was actively performed hip and knee flexion exercises on the bed. No weight-bearing on the affected limb. Encourage able patients to bear part of the weight on the affected limb within the tolerable range 4 weeks after operation. Gradually walk with a walker with weight-bearing according to the X-ray follow-up at 6 to 8 weeks. Patients who cannot walk independently and have severe osteoporosis For patients with continuous bone callus growth on X-ray, they can gradually walk with weight bearing under the support.
Contact Person: Yoyo (Product Manager)
TEL/Whatsapp: +86 15682071283