Volar Plate for Distal Radius Fractures, Basics, Practicality, Skills, Experience!
At present, there are various treatment methods for distal radius fractures, such as plaster fixation, open reduction and internal fixation, external fixation frame, etc. Among them, volar plate fixation can obtain a more satisfactory effect, but there are reports in the literature that its complications are as high as 16%. However, if the steel plate is selected properly, the incidence of complications can be effectively reduced. This paper briefly summarizes the characteristics, indications, contraindications, and surgical techniques of volar plate treatment of distal radius fractures.
1. There are two main advantages of the palm side plate
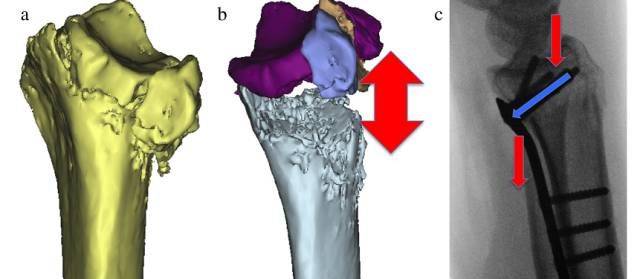
A.It can neutralize the component of buckling force. Fixation with angled fixation screws supports the distal fragment and transfers the load to the radial shaft (Fig. 1). It can obtain subchondral support more effectively. This plate system can not only stably fix distal intra-articular fractures, but also can effectively restore the anatomical structure of intra-articular subchondral bone through peg/screw "fan-shaped" fixation. For most distal radius fracture types, this roof system provides increased stability allowing early mobilization.
Picture 1, a, after three-dimensional reconstruction of a typical comminuted distal radius fracture, pay attention to the degree of dorsal compression; b, virtual reduction of the fracture, the defect must be fixed and supported by a plate; c, lateral view after DVR fixation, the arrow indicates load transfer .
B.Less impact on soft tissue: volar plate fixation is slightly below the watershed line, compared with the dorsal plate, it can reduce the irritation to the tendon, and there is more available space, which can more effectively avoid the implant and tendon. direct contact. Additionally, most implants can be covered by the pronator quadratus.
2. Indications and contraindications for the treatment of distal radius with volar plate
a.Indications: For the failure of closed reduction of extra-articular fractures, the following conditions occur, such as dorsal angulation greater than 20°, dorsal compression greater than 5mm, distal radius shortening greater than 3mm, and distal fracture fragment displacement greater than 2mm; The displacement of the internal fracture is greater than 2 mm; due to the low bone density, it is easy to cause re-displacement, so it is relatively more suitable for the elderly.
b. Contraindications: use of local anesthetics, local or systemic infectious diseases, poor skin condition on the volar side of the wrist; bone mass and fracture type at the fracture site, dorsal fracture type such as Barton fracture, radiocarpal joint fracture and dislocation, simple radius Styloid process fracture, small avulsion fracture of volar margin.
For patients with high-energy injuries such as severe intra-articular comminuted fractures or severe bone loss, most scholars do not recommend the use of volar plates, because such distal fractures are prone to vascular necrosis and difficult to obtain anatomical reduction. For patients with multiple fracture fragments and significant displacement and severe osteoporosis, volar plate is difficult to be effective. There may be problems with subchondral support in distal fractures, such as screw penetration into the joint cavity. A recent literature reported that when 42 cases of intra-articular fractures were treated with volar plates, no articular screws penetrated into the articular cavity, which was mainly related to the position of the plates.
3. Surgical skills
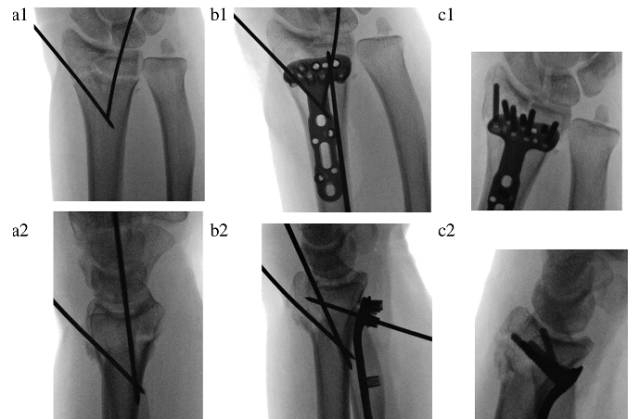
Most physicians use volar plate fixation for distal radius fractures in similar ways and techniques. However, to effectively avoid the occurrence of postoperative complications, a superb surgical technique is required, for example, the reduction can be obtained by releasing the compression of the fracture block and restoring the continuity of the cortical bone. Temporary fixation with 2-3 Kirschner wires can be used. Regarding which approach to use, the author recommends PCR (flexor carpi radialis) to extend the volar approach.
a, Temporary fixation with two Kirschner wires, note that the volar inclination and articular surface are not fully restored at this time;
b, A Kirschner wire temporarily fixes the plate, pay attention to the fixation of the distal end of the radius at this time (distal fracture fragment fixation technique), the proximal part of the plate is pulled toward the radial shaft to restore the volar inclination.
C, The articular surface is fine-tuned under arthroscopy, the distal locking screw/pin is placed, and the proximal radius is finally reduced and fixed.
Key points of approach: The distal skin incision starts at the skin fold of the wrist, and its length can be determined according to the type of fracture. The flexor carpi radialis tendon and its sheath are dissected distal to the carpal bone and as proximal as possible. Pulling the flexor carpi radialis tendon to the ulnar side protects the median nerve and flexor tendon complex. The Parona space is exposed, with the pronator quadratus located between the flexor hallucis longus (ulnar) and the radial artery (radial). Incision was made on the radial side of the pronator quadratus, leaving a part attached to the radius for later reconstruction. Pulling the pronator quadratus to the ulnar side more fully exposes the volar ulnar angle of the radius.
For complex fracture types, it is recommended to release the distal insertion of the brachioradialis muscle, which can neutralize its pull on the radial styloid process. At this time, the volar sheath of the first dorsal compartment can be cut to expose the distal fracture Block the radial side and radial styloid process, internally rotate the radial shaft to separate from the fracture site, and then use Kirschner wires to reduce the intra-articular fracture block. For complex intra-articular fractures, arthroscopy can be used to assist reduction, assessment, and fine-tuning of the fracture fragments.
After the reduction is completed, the volar plate is routinely placed. The plate must be just close to the watershed, must cover the ulnar process, and the proximal end of the plate should reach the midpoint of the radial shaft. If the above conditions are not met, the plate size is not suitable, or the reduction is not satisfactory, the operation is still not perfect.
Many complications have a lot to do with where the plate is placed. If the plate is placed too radially, complications related to the flexor hallucis longus are predisposed; if the plate is placed too close to the watershed line, the flexor digitorum profundus may be at risk. Fracture reduction to the volar displacement deformity may easily cause the steel plate to protrude to the volar side and directly contact the flexor tendon, eventually leading to tendinitis or even rupture.
For osteoporotic patients, it is recommended that the plate be as close to the watershed line as possible, but not across it. Kirschner wires can be used to fix the subchondral closest to the ulna, and the side-by-side Kirschner wires and locking nails and screws can effectively prevent the fracture from redisplacement.
After the plate is placed correctly, the proximal end is fixed with a screw, and the ulnar hole at the far end of the plate is temporarily fixed with a Kirschner wire. Intraoperative fluoroscopy anteroposterior view, lateral view, wrist joint elevation 30° lateral view, to determine fracture reduction and internal fixation position. If the position of the plate is satisfactory, but the Kirschner wire is in the joint, it will lead to insufficient recovery of the volar inclination, which can be solved by resetting the plate through the "distal fracture fixation technique" (Fig. 2, b).
If it is accompanied by dorsal and ulnar fractures (ulnar/dorsal Die Punch) and cannot be fully reduced under closure, the following three techniques can be used:
1. Pronate the proximal end of the radius to keep it away from the fracture site, and push the lunate fossa fracture towards the carpus through the PCR extension approach;
2. Make a small incision on the dorsal side of the 4th and 5th compartment to expose the fracture fragment, and fix it with screws in the most ulnar hole of the plate.
3. Closed percutaneous or minimally invasive fixation with the aid of arthroscopy.
After the reduction is satisfactory and the plate is placed correctly, the final fixation is relatively simple. If the proximal ulnar Kirschner wire is positioned correctly and no screws are in the joint cavity, an anatomical reduction can be obtained.
Screw selection experience: Due to the severe comminution of the dorsal cortical bone, the length of the screw may be difficult to measure accurately. Screws that are too long may cause irritation of the tendon, and screws that are too short cannot support and fix the dorsal fragment. For this reason, the author recommends using threaded locking screws and multiaxial locking screws in the radial styloid process and the most ulnar hole, and using polished rod locking screws in the rest of the positions. Using a blunt tip avoids irritation of the tendon even if the dorsal exit is used. For proximal interlocking plate fixation, two interlocking screws + one ordinary screw (placed through the ellipse) can be used for fixation.
4. Summary of the full text:
Volar locking nail plate fixation of distal radius fractures can achieve good clinical efficacy, which mainly depends on the selection of indications and superb surgical skills. Using this method can get better early functional prognosis, but there is no difference in later function and imaging performance with other methods, the incidence of postoperative complications is similar, and the reduction is lost in external fixation, percutaneous Kirschner wire fixation, and plaster fixation , needle tract infections are more common; and extensor tendon problems are more common in distal radius plate fixation systems. For patients with osteoporosis, the volar plate is still the first choice.